intussusception treatment in adults
 Factors predicting malignancy in adult intussusception: An experience in university-affiliated hospitals - ScienceDirect
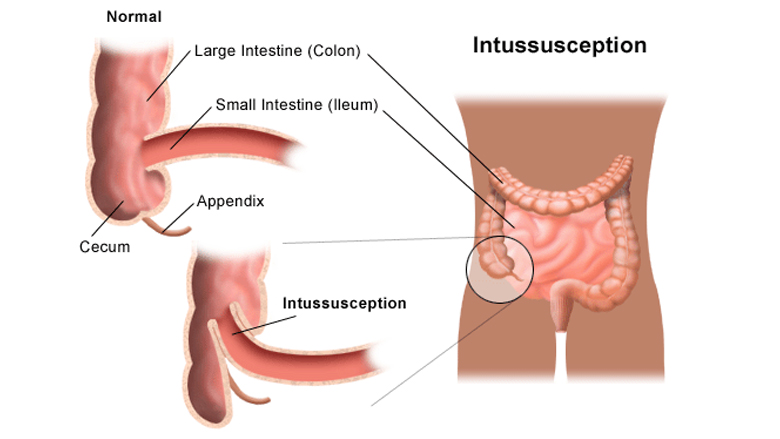
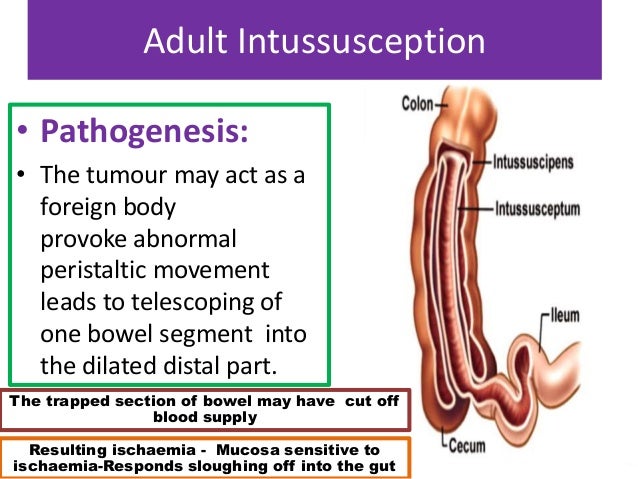
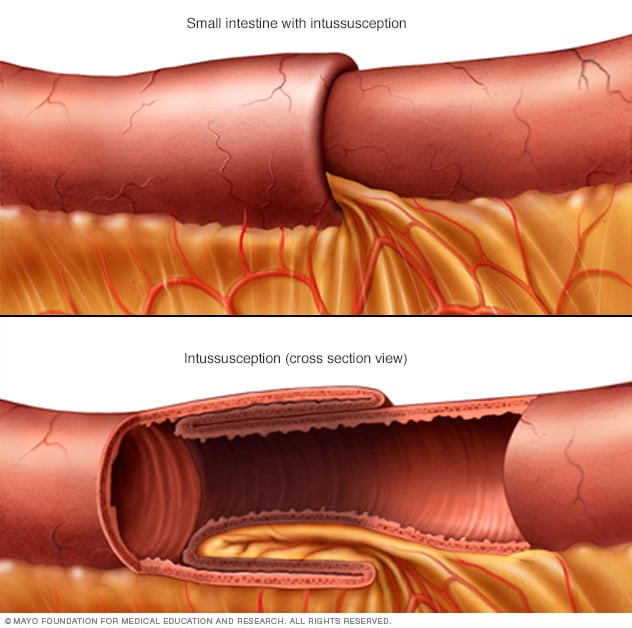
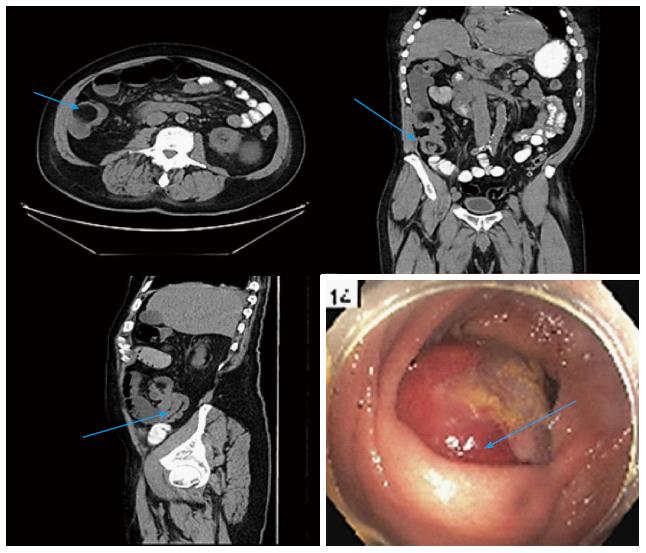
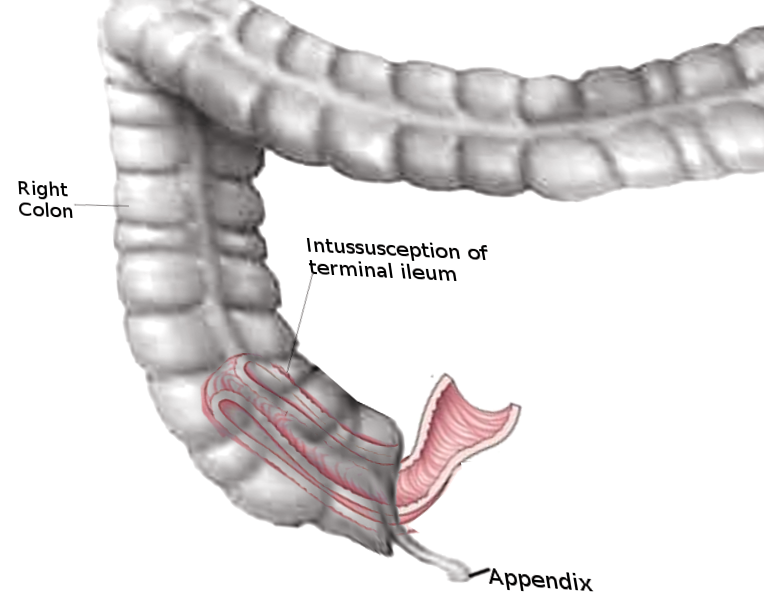
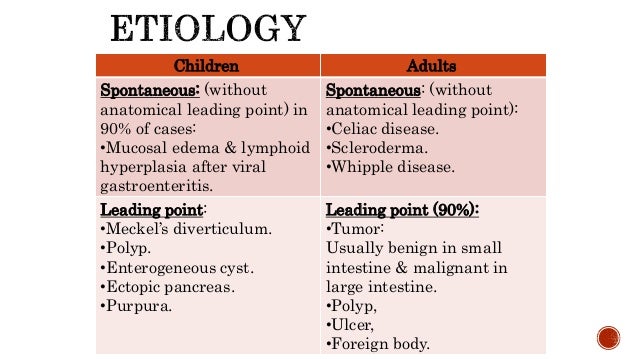
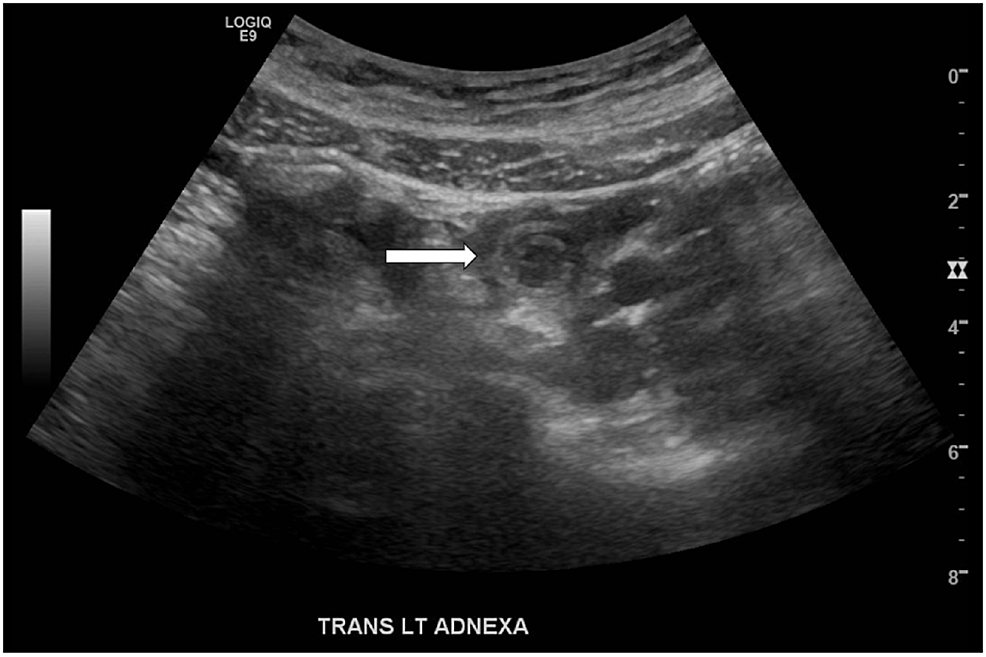
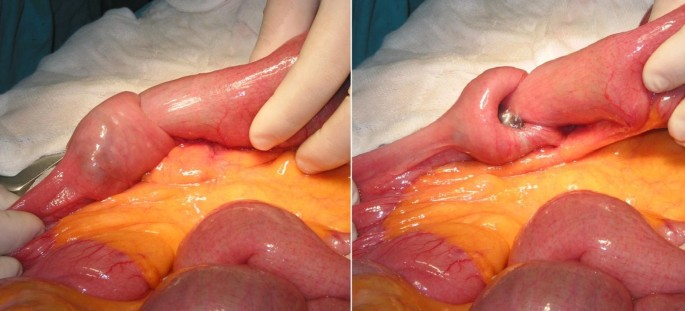
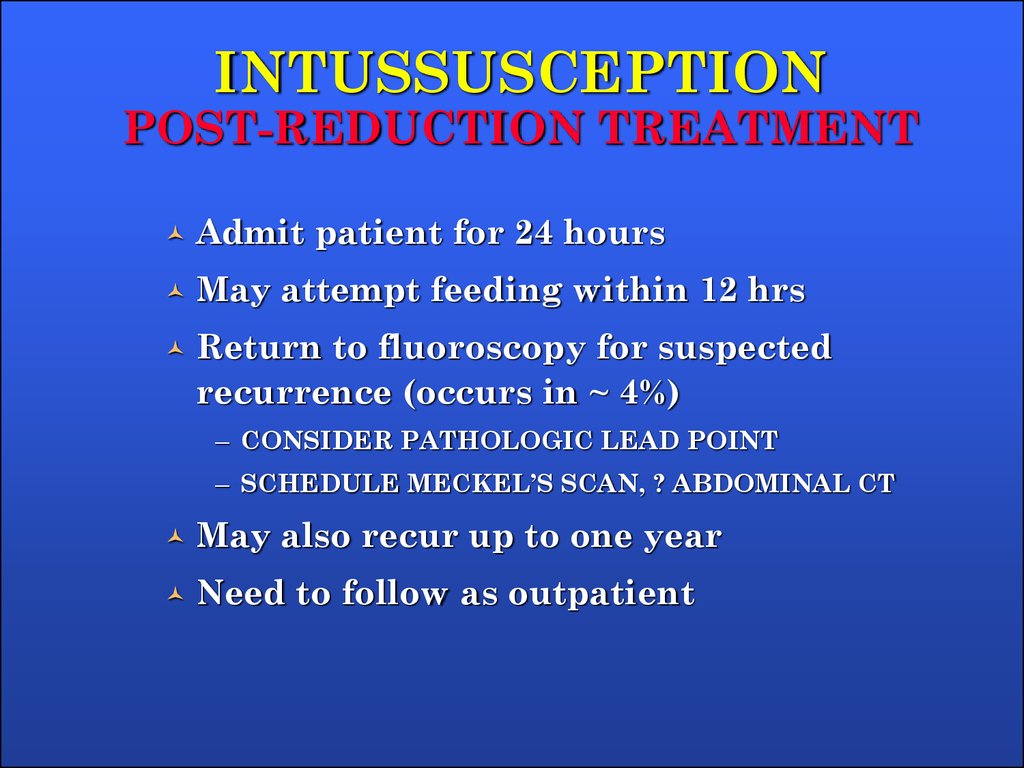
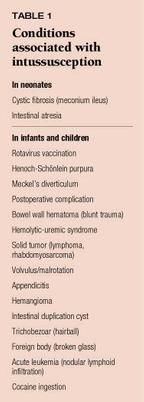
Factors predicting malignancy in adult intussusception: An experience in university-affiliated hospitals - ScienceDirectJavaScript is currently disabled, this site works much better if you enable JavaScript in your browser. *indicates required fields Case reports in GastroenterologySingle Case Intususception in adults: Think of cancer! Hadid T.a,b · Elazzamy H.c · Kafri Z.a, b aDepartment of Internal Medicine, Wayne State University School of Medicine, Detroit, MI, USAbDepartment of Internal Medicine, Ascension St. John Hospital, Detroit, MI, USAcGraduate Medical Education, Department of Pathology and Laboratory Medicine, Ascension St. John Hospital, Detroit, MI, USA Tarik Hadid, MD, MPH, MSDepartment of Internal Medicine, Wayne State UniversitySchool of Medicine, 540 E Canfield StreetDetroit, MI 48201 (USA)E-Mail thadid@wayne.edu Keywords: Related articles for "" Intususception in adults: Think of cancer! Tarik Hadid, MD, MPH, MSDepartment of Internal Medicine, Wayne State UniversitySchool of Medicine, 540 E Canfield StreetDetroit, MI 48201 (USA)E-Mail thadid@wayne.eduKeywords: Related Articles for "ResumenIntususception is a rare phenomenon in adults and usually presents with intestinal obstruction. Unlike childhood intususception, adult intususception is rarely idiopathic and is often associated with secondary causes such as benign and malignant tumors. While most cases are treated surgically, emerging data suggest a more conservative approach to management for patients with short-segment adult intussusception and without high-risk features such as intestinal obstruction, mass imaging, colon involvement or constitutional symptoms of malignancy. We present a rare case of adult intususception due to non-supposed adenocarcinoma of the jejune, successfully treated with surgical resection followed by adjuvant chemotherapy. We favor the surgical approach rather than conservative for adult patients with intussception to avoid unsuspecting malignant tumors that are not easily visualized in imaging studies.© 2020 The author(s). Published by S. Karger AG, Basel IntroductionThe intususception of the towel represents a rare type of intestinal obstruction and is defined as telescoping the proximal loop of the intestine (intussusceptum) within the distal loop (intussuscipiens), which results in the obliteration of the lumen [, ]. While it is commonly found in children, adult intususception (AI) is extraordinarily rare, with an estimated incidence of 2 cases/1,000,000 population/year [, ]. Childhood intussception is commonly idiopathic (primary) with most cases related to the ileum but may rarely involve the stomach, colon, and the rest of the small intestine. It occurs more commonly in male children between 4 and 10 months old [, , ]. Curiously, the tetravalent rotavirus vaccine is associated with a slightly higher risk of intususception among vaccinated children (1.5 cases of excess per 100,000) []. On the other hand, AI is associated with underlying pathology (secondary) in 90% of cases and equally affects men and women [, ]. AI is presented in the small intestine in 52% of cases and the large intestine in 38% with 10% involving the stomach and surgical stomach [, ]. The clinical symptoms of AI are variable and often not specific. Patients may have diffuse abdominal pain, nausea, vomiting, blood feces, changes in bowel habits and/or abdominal distended. The clinical test may reveal abdominal discontinuation or diffuse abdominal tenderness, but often does not show any anomaly. The ambiguity of these clinical findings and their similarity with many other more common conditions such as inflammatory bowel diseases, intestinal obstruction due to peritoneal adhesions, and infectious gastroenteritis make the clinical diagnosis of the AI quite challenging. Diagnosing AI requires a high suspicion rate, which often requires the use of imaging studies such as computerized tomography (CT) []. It should be noted that the generalized medical use of CT has increased the preoperative diagnosis rate of AI []. While more than 80% of cases in children can be reduced with hydrostatic enemas, most cases of AI require surgical intervention [, , ]. Untreated intususception can be life-threatening, starting with progressive intestinal distention, which in turn produces an increase in intralumec pressure, which eventually leads to microvascular ischemia, thysular necrosis with subsequent intestinal perforation, and peritonitis []. Therefore, early diagnosis and treatment of AI are critical to avoid these complications. In this report, we present a case of AI due to the underlying malignant jejunal neoplasm that was effectively diagnosed and treated. We also discuss some of the diagnostic procedures and therapeutic interventions used in the management of the AI. Case presentationA 69-year-old non-diabetic female presented with altered mental state, nausea, vomiting and diffuse abdominal discomfort for 3 days. He did not report hematochezia or melena, but he admitted poor appetite and 20 pounds of weight loss in the last 6 months. His past medical history was positive for atrial fibrillation, rheumatoid arthritis, chronic obstructive pulmonary disease and hyperthyroidism. He had a history of iron deficiency anemia for 2 years with hemoglobin nadir of 7.4. Esophagogastroduodenoscopia and colonoscopy performed 2 years before the presentation did not reveal any source of bleeding. The patient was treated with oral iron supplement with hemoglobin enhancement at 11.7. I had no previous abdominal surgery. It smoked 5 to 9 cigarettes a day for more than 20 years but denied drinking alcohol or using illicit drugs. He didn't report a family history of malignity. The test revealed blood pressure of 139/70, pulse of 91/min, temperature of 97.6°F, oxygen saturation of 100% in the room air, and weight of 120 pounds. Your head and neck exam revealed mild exophthalmos without cervical or supraclavicular lymphadenopathy. Pulmonary and heart tests were normal. The abdomen was moderately neglected with diffuse tenderness, and its limbs had no edema. In the presentation, the complete blood count (CBC) showed a white blood cell count of 5,100/μL, hemoglobin of 8.4 g/dL, average corpuscular volume of 81.9 fl and platelet count of 172,000/μ L. CBC 1 year earlier showed hemoglobin of 10 g/dL. When admitted, it was found that it had glucose of 41 mg/dL (secondary only to decrease oral intake), which was successfully treated by intravenous dextrose. After improving the mental state and administration of proper hydration, a CT scan of the abdomen and pelvis was performed and high-grade intestinal obstruction was revealed due to the intususception of small intestine (Fig. ). A transition point was identified in the media-pelvis, but no mass could be seen. Laparotomy confirmed intususception (Fig. ), and 10 cm of the mid-jejune were resected. Moderately differentiated, invasive 5 cm invasive adenocarcinoma with focal areas of necrosis (Fig. ). There was no evidence of lymphedical invasion. All surgical margins were negative, and only one in three resected lymph nodes was positive. A CT scan of the chest did not reveal evidence of metastatic disease. It was staged as T3N1M0 (phase III). After recovering from the operation, he received 12 cycles of adjuvant chemotherapy with 5-fluorouracil, leucovorina and oxaliplatin, which tolerated well. Repeating computed tomography after the termination of therapy did not reveal evidence of recurrence. Repeating CBC was normal with hemoglobin of 14.1 g/dL. She's still alive without disease evidence 2 years after the initial presentation. TC of the pelvis showing small intestinal intususception. Operating image showing intususception of the jejune. Hematoxylin and stained section of resected jejunium eosin that shows malignant cells forming gland, consistent with adenocarcinoma (magnification ×40). Debate AI is a rare clinical entity with potential for serious complications if not recognized and treated quickly. It is often classified on the basis of its location to entero-enteric (confined to the small intestine), colo-colic (confined to the large intestine), ieo-colic (when the terminal ileum is submerged to the ascending colon), and ieo-cecal (when the ileo-cecal valve is the main point of intussception) []. It can also be classified based on its etiology for benign, malignant and idiopathic. More than 90% of pediatric cases are idiopathic []. The hypertrophy of lymph tissues in the terminal ileum, known as the Peyer patch, is thought of the main point of intussception in children and can be triggered by viral infections []. On the other hand, the etiology of the AI includes carcinoma, Meckel diverticulum, colon diverticulum, lymphoma, lipoma, rigures, metastatic lesions, polyps or inflammatory lesions. Adenocarcinoma accounts for 30% of all intusions of small adult intestines and 66% of colonic intususions [, ].The classic presentation of childhood intususception, which includes the triad of coconut abdominal pain, rantin stool and a flexible abdominal mass in the form of sausage, is rarely found in adults. Most patients have symptoms and signs of intestinal obstruction. Although symptoms usually occur acutely, they may be under- or chronic, especially in colon intususception. In children, the abdominal ultrasound provides a rapid and sensitive screening test for intussception and can reveal the "doughnuts' sign" and the "pseudo-kidney apparition" []. In adults, it was found that computed tomography was more accurate []. In a study, it was reported that the diagnostic accuracy of computed tomography was almost 100% [, ]. The appearance of TC usually includes a "object", "yellow of the wrist", or sausage-shaped lesions. Alternatively, it was found that ultrasound was less reliable in adults, due to intestinal edema, airflow levels and larger fecal charges []. The treatment modalities for intususception are variable. Because ieo-colic is the most common type seen in children, the reduction is often successful by using pneumatic or hydrostatic edema. In addition, integer-enteric intusions generally reduce spontaneously. Alternatively, AI is treated historically surgically. Random clinical trials are missing that compare operational and non-cooperative approaches to AI. However, a recent study suggested that up to 82% of radiological intusions can be treated safely and successfully. However, this approach should be used with great caution to prevent potentially serious underlying conditions such as malignancy. The operational approach is necessary in patients with intestinal obstruction, those with mass view by image, those with constitutional symptoms of malignancy (such as weight loss, anorexia, night sweating, etc.), and those with colobolic and ieocholic intussception (due to their superior association with malignity) []. Adults with integer-enteric intusions shorter than 3.5 cm and without any of the above features are often self-limiting and can be considered for non-operational management []. Our patient was treated surgically, as he presented a small bowel obstruction and had a significant weight loss (14% of his body weight); both were related to underlying malignancy. When surgery is performed, intususception should be surgically reduced in children and resected in adults. If it is suspected that there is underlying malignancy, the oncological resection in the block of the involved intestine and associated mesentry should be sought. In colobolic intusions, preoperative colonoscopy may be useful in identifying underlying pathology and may help in appropriate surgery planning. However, colon biopsy should be performed with caution due to the increased risk of perforation due to tissue ischemia []. The IA prognosis depends to a large extent on the underlying pathology. If malignity is found, appropriate antineoplastic therapy should be instituted postoperatively if clinically indicated. In conclusion, AI can be a manifestation of serious conditions such as malignancy. While conservative management was proposed in low-risk patients, we favor the surgical approach to avoid potentially curable malignancy as in our patient. Oncology surgery and subsequent antineoplastic therapy should be used to make these patients optimise clinical outcomes. Ethical Statement The patient provided written consent for publication. He was provided with a copy of the manuscript. Dissemination Statement All authors reveal that they do not have conflicts of interest related to this study. Sources of funding The authors received no funding. Author's contributions Tarik Hadid, MD, MPH, MS, obtained the patient's consent, patient care, collected the patient's data, revised the literature, wrote the initial draft of the manuscript, and revised the later versions. Haidy Elazzamy, MD, reviewed the pathology of the resected specimen, prepared the pathological figure for the manuscript, and revised and edited the manuscript. Zyad Kafri, MD, MS, revised, edited and supervised the process of building the manuscript to its final version. Related Articles:References Author ContactsTarik Hadid, MD, MPH, MSDepartment of Internal Medicine, Wayne State UniversitySchool of Medicine, 540 E Canfield StreetDetroit, MI 48201 (USA)E-Mail thadid@wayne.eduArticle/Publication Details Received: November 03, 2019 Accepted: December 17, 2019 Published online: January 20, 2020 Date of publication: January - April Number of printing pages: 7 Number of figures: 3 Number of tables: 0 eISSN: (Online) For additional information: Open Access License / Drug Dosage / Exemption This article is licensed under the Creative Commons Attribution-NoCommercial 4.0 International License (CC BY-NC). Use and distribution for commercial purposes requires written permission. Drug Dosage: The authors and the editor have made every effort to ensure that the selection and dosage of drugs set out in this text are in accordance with current recommendations and practices at the time of publication. However, in view of the ongoing investigation, changes in government regulations and the steady flow of information concerning drug therapy and drug reactions, the reader is urged to review the insert of packages for each drug for any change in indications and doses and for additional warnings and precautions. This is particularly important when the recommended agent is a new medication and/or employee infrequently. Disclaimer: The statements, opinions and data contained in this publication are only those of the authors and individual collaborators and not of the editors and editors. The appearance of advertisements or/and product references in the publication is not a guarantee, approval or approval of the products or services announced or their effectiveness, quality or safety. The editor and the editor(s) claim liability for any damage to persons or property resulting from any idea, method, instructions or products to which the content or advertisements relates. References 2020, Vol.14, January-April Article Silence Karger International: Silence Silence © 2021 S. Karger AG, Basel Silence Silence Karger International: Silence Silence Silence Silence © 2021 S. Karger AG, BaselSign up for MyKarger Manage with MyKarger your orders quickly and easily, save your favorite items on your reading list, edit your newsletter profile and enjoy attractive discounts. This site is protected by reCAPTCHA and Google and applies. Set your password Your password must comply with the following rules: Get in MyKarger? We found an existing MyKarger account with this email address: Complete your name Thank you for registering Your MyKarger account has been created. Please check your emails to validate your email address. Restore Your Password To reset your password, enter your email address or your user ID with which you registered. You will be sent an email containing a link to reset your password. Check your E-Mails A link has been sent to reset your password to your email address. Follow the instructions and try to log in again.
View of Adult intussusception: a six-year experience at a single center | Annals of Gastroenterology

Differences between adult and childhood intussusceptions | Download Table

Figure 10 from Lesion Stomach Small Bowel Large Bowel Benign Adenoma Leiomyoma Lipoma Hamartoma Inflammatory polyps Lipoma | Semantic Scholar
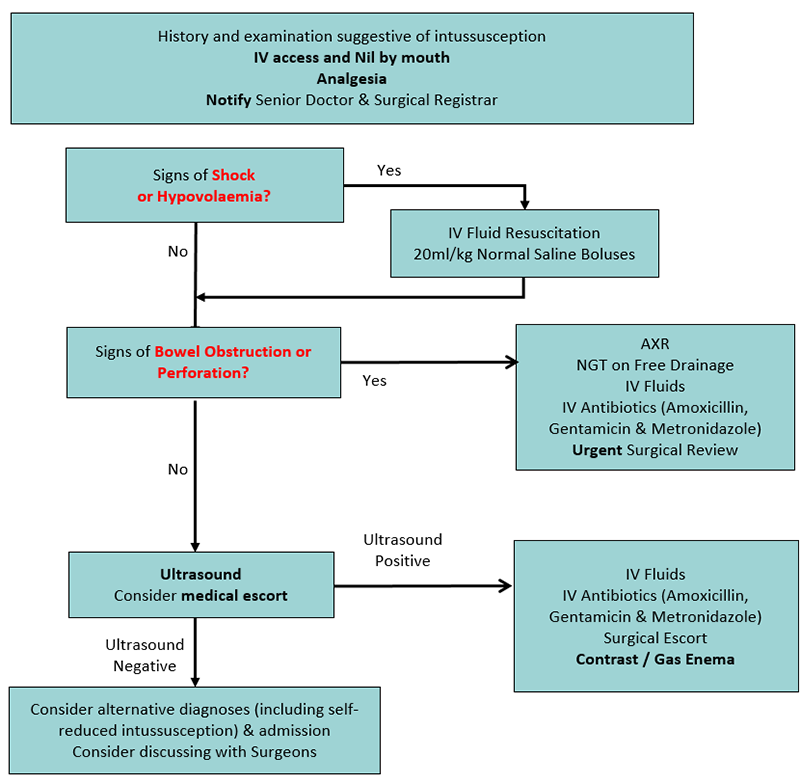
Clinical Practice Guidelines : Intussusception

Intussusception: Treatment, Causes, Symptoms, Risk Factors, Tests
Intussusception (Bowel Obstruction): Treatment & Symptoms
Intussusception in Adults

Laparoscopic Treatment of Chronic Small Bowel Intussusception Due to Meckel's Diverticulum in an Adult Male - SAGES Abstract Archives

Adult intussusception - ppt video online download
Intussusception | Children's Hospital of Philadelphia
A Rare Case of Adult Intussusception Treated by Laparoscopic Assisted Surgery
Intussusception in Adults-Submucosal Lipoma at Transverse colon-A ra…
emDOCs.net – Emergency Medicine EducationAdult Intussusception: Not Like Trix, Not Just for Kids - emDOCs.net - Emergency Medicine Education
Intussusception - Symptoms and causes - Mayo Clinic

Intussusception (medical disorder) - Wikipedia

Figure 11 from Lesion Stomach Small Bowel Large Bowel Benign Adenoma Leiomyoma Lipoma Hamartoma Inflammatory polyps Lipoma | Semantic Scholar
View of Adult intussusception: a six-year experience at a single center | Annals of Gastroenterology
Adult intussusception: A case series and review

Proposed decision tree for management of adult patients with... | Download Scientific Diagram
Intussusception In Adults Article

Surgical versus conservative management of adult intussusception: Case series and review - ScienceDirect

Adult Incidental Intussusception - Single Institute Experience - SAGES Abstract Archives

Presentation, aetiology and treatment of adult intussusception in a tertiary Sub-Saharan Hospital: a 10-year retrospective study – topic of research paper in Clinical medicine. Download scholarly article PDF and read for free

Intussusception Treatment with Ayurvedic Herbal Remedies
Intussusception
What is Intussusception in adults? - Dr. Nagaraj B. Puttaswamy - YouTube

Adult Intestinal Intussusception: CT Appearances and Identification of a Causative Lead Point | RadioGraphics

Intussusception of the bowel in adults: A review
Cureus | Adult Small Bowel Intussusception and Resolution Captured on Pelvic Ultrasound
Intussusception of the small bowel secondary to malignant metastases in two 80-year-old people: a case series | Journal of Medical Case Reports | Full Text

Laparoscopic Management of Intussusception in an Adult - SAGES Abstract Archives
Intussusception definition - online presentation
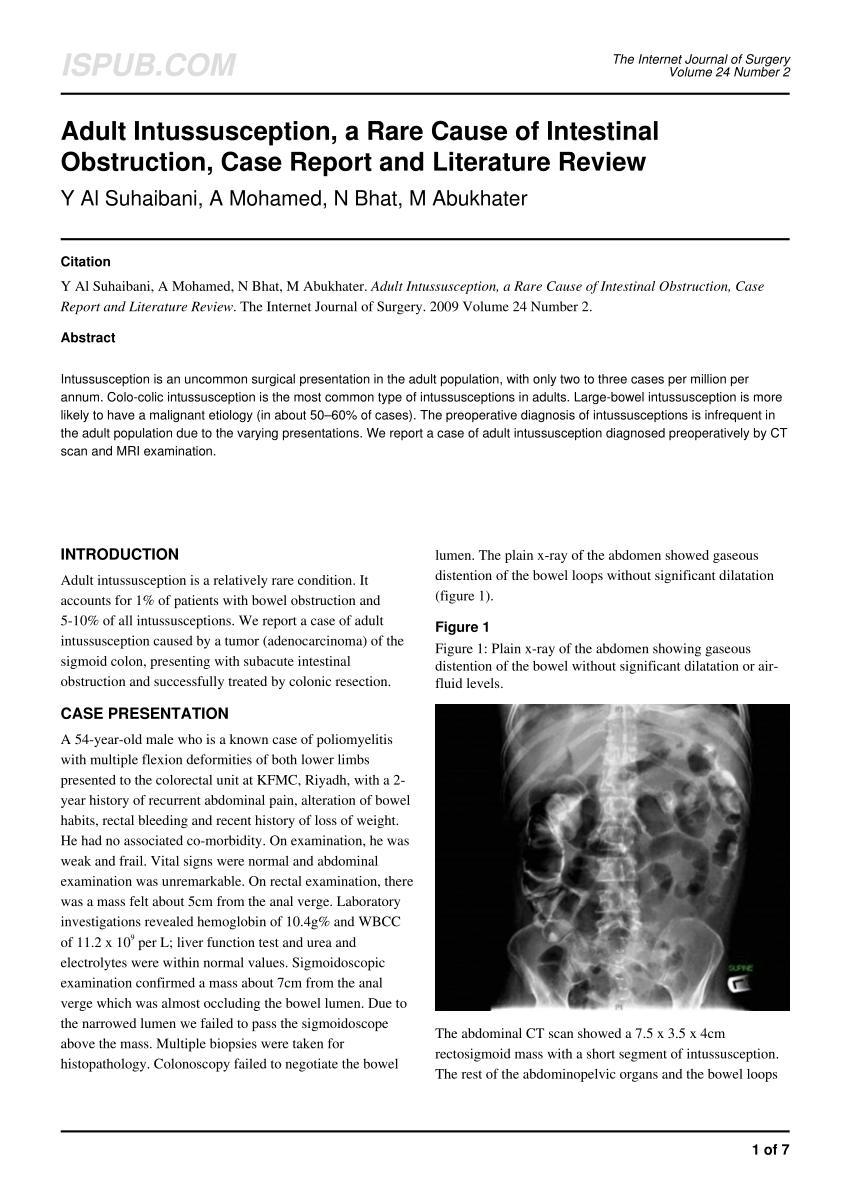
PDF) Adult Intussusception, a Rare Cause of Intestinal Obstruction, Case Report and Literature Review

Intussusception in adults

Intussusception Symptoms, Treatment, Surgery, Diet, Success

Adult intussusception: case reports and review of literature | Postgraduate Medical Journal
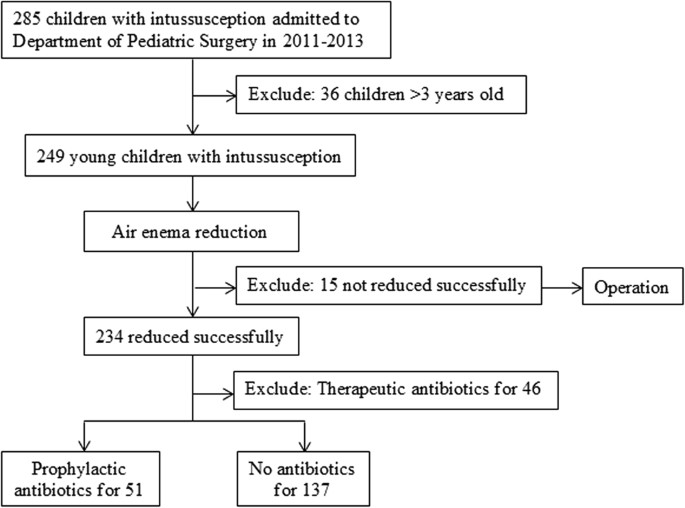
No Prophylactic Antibiotic Use for Young Children's Intussusception with Low-risk Infection after Successful Air Enema Reduction | Scientific Reports
Update on intussusception
emDOCs.net – Emergency Medicine EducationAdult Intussusception: Not Like Trix, Not Just for Kids - emDOCs.net - Emergency Medicine Education

Idiopathic small-bowel intussusception in an adult | CMAJ
Posting Komentar untuk "intussusception treatment in adults"